INTRODUCTION AND BACKGROUND
Among the highest COVID-19-associated morbidity and mortality rates in the United States are found in non-Native Hawaiian Pacific Islanders (PI), defined as the indigenous people of the three territories of the U.S. Affiliated Pacific Islands (Guam, Commonwealth of the Northern Mariana Islands, and American Samoa) and persons of the sovereign nations that have a Compact of Free Association treaty with the U.S. (the Federated States of Micronesia, Republic of the Marshall Islands, and Republic of Palau). PI also suffer from higher rates of medical co-morbidities (obesity, hypertension, diabetes, cardiovascular disease) known to increase the risk of poor COVID-19 outcomes. Moreover, PI suffer from poor access to health care, lack medical insurance, live in multi-generational, overcrowded housing, and have low-paying service jobs that put them in frequent contact with the infected public. Hawaii is now experiencing another surge in COVID-19, with a doubling of positive SARS-CoV-2 diagnostic tests from 1% to 2%. From the very onset of COVID-19 in Hawaii, PI have been disproportionately affected, leading all other ethnic groups. The latest figures, available from the Hawaii Department of Health on May 3, 2021, show that while PI comprise only 4% of the State’s population, they account for 20% of COVID-19 cases (Fig. 1), 29% of COVID-19 hospitalizations (Fig. 2), and 22% of COVID-19 deaths (Fig. 3). Of great concern is that many of the COVID-19 cases are among individuals younger than 50 years of age (Fig. 4). On Guam, indigenous CHamoru and immigrant Micronesians represent the majority of COVID-19 cases. These underserved PI communities are in urgent need of culturally appropriate COVID-19 response measures.

Fig 1. COVID-19 cases by ethnicity in Hawaii
Disproportionate number of COVID-19 cases among PI.
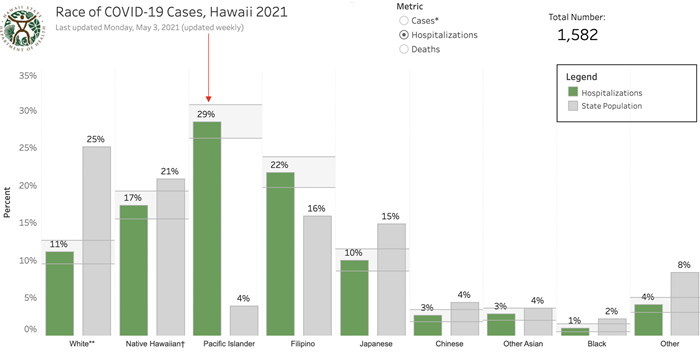
Fig. 2. COVID-19 hospitalizations by ethnicity in Hawaii
Disproportionate number of hospitalizations among PI.
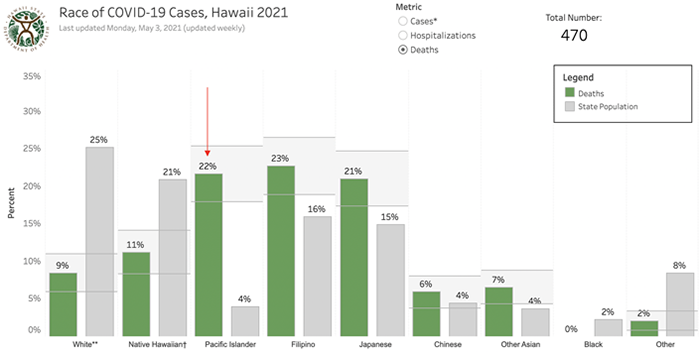
Fig 3. COVID-19 deaths by ethnicity in Hawaii
Disproportionate number of COVID-19 deaths among PI.
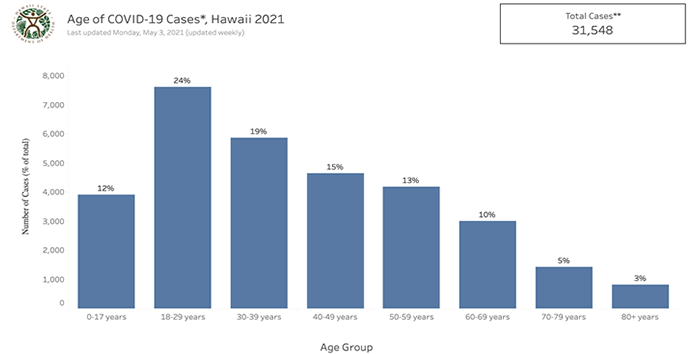
Fig. 4. COVID-19 cases by age in Hawaii
More than 50% of all cases are in people younger than 50 years.
Long before the COVID-19 pandemic, PI have been largely invisible and overlooked in the socio-economic fabric and healthcare infrastructure in Hawaii. They have suffered generations-long historical trauma from discrimination, implicit bias, colonialism and poverty. Alarmingly, in recent COVID-19 response efforts, a National Academies draft document on COVID-19 vaccine allocation strategies aimed at racial/ethnic disparities groups does not even mention PI (T. Nguyen, personal communication, 2020). In Hawaii (population, 1,455,271), PI communities have disproportionately borne the brunt of COVID-19. On Guam (population, 168,775), the western-most U.S. territory in the Pacific, the COVID-19 has also predominantly affected the indigenous CHamoru and immigrant Micronesians.