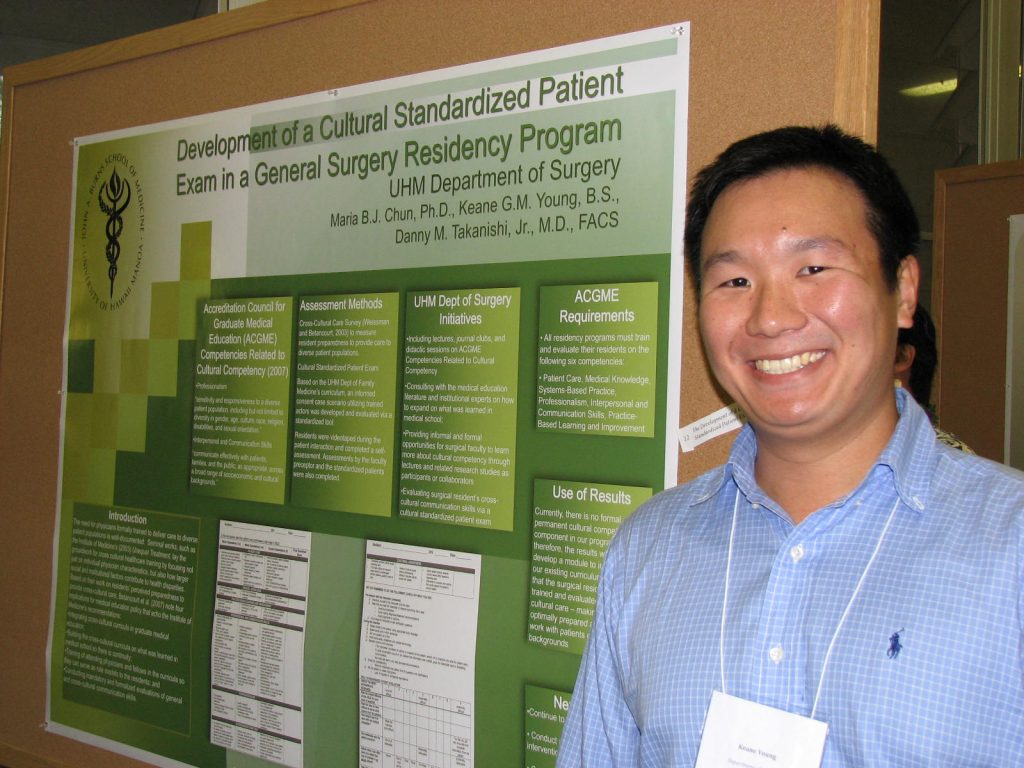
Due to the growing diversity of the United States population, various legal mandates and accrediting bodies require doctors to receive training that will allow them to provide optimal care to patients regardless of their cultural backgrounds. More prevalent in medical specialties such as family medicine and psychiatry, the inclusion of cultural competency or cross-cultural care issues in surgery is an emerging area of recognized need. A nationwide survey on residents’ perceptions of their preparedness to provide cross-cultural care revealed that surgical residents view cultural knowledge as important, but were hampered in acquiring these skills due to a lack of time and absence of formal training. The Accreditation Council for Graduate Medical Education requires residency programs to incorporate cultural training into their curricula. Of the six competencies, cultural competency is addressed under both Professionalism and Interpersonal and Communication Skills. With the assistance of the UH Department of Family Medicine and Community Health, the UH Department of Surgery’s general surgery residency program has developed and is currently piloting a cultural standardized patient exam as a means to both train and evaluate its residents. The case scenario involves a surgeon attempting to obtain informed consent from an elderly Samoan male who needs to have his leg amputated or face certain death. All Program Year-1 (PGY-1) residents (n=13) participated in the exam and were evaluated by one of four faculty preceptors using a standardized tool. Using this as the baseline, an educational training intervention is being planned, which will be followed by a post-test. By Maria B.J. Chun, Ph.D., Keane G.M. Young, B.S., Danny M. Takanishi, Jr., M.D., FACS
Recommended Citation:
Chun, M., Young, Keane G., Takanishi, D. (2009, December). The Development of a Cultural Standardized Patient Exam for a General Surgery Residency Program. Poster session presented at the Assessment for Curricular Improvement Poster Exhibit at the University of Hawai’i at Mānoa, Honolulu, HI.
